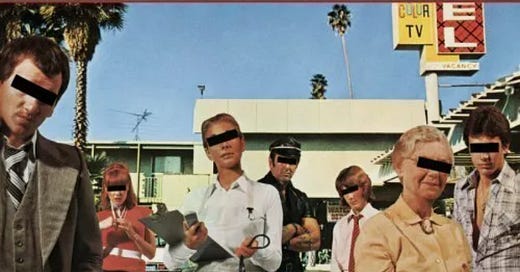
Dirty Deeds Done Dirt Cheap
Our 'cheap trick' paper is rejected by a mainstream journal, confirming that captured peer review survives unabated
Readers will be familiar with our efforts to expose the nefarious and commonplace practice of intentionally miscategorising those vaccinated against covid as unvaccinated if they contract ‘covid’, despite receiving a vaccine, or suffer a side effect or die of the vaccine within (usually) 14 days of vaccination. The motivation for employing the cheap tri…
Keep reading with a 7-day free trial
Subscribe to Where are the numbers? by Norman Fenton and Martin Neil to keep reading this post and get 7 days of free access to the full post archives.