WTF Happened to Influenza in 2020-2021?
Using the surveillance data from Canada Public Health, exploring the interaction between Influenza and SARS-CoV-2, and the science behind PCR testing, we've stumbled upon a problem.
Mysterious Case of the Disappearing Flu
Once the world lost its mind from the SARS-CoV-2 outbreak in Spring of 2020, myself and several others started to ask “Where’s influenza?” For a good chunk of time (March-September of 2020) this was not that important, as the flu season starts to kick off in October in the northern hemisphere.
During the winter of 2020-2021, the flu season came and went with rather little attention as the world was focused on vaccine distribution followed swiftly by concerns of the Delta variant.
Given Canada’s relatively small population, centralized medical information, and regular monitoring of influenza we will use the Canadian Communicable Disease Report to explore this mystery.
Canadian National Influenza Annual Report
Before we dive into the 2020-2021 data, let’s look at a season preceding COVID-19. The following figure is from the 2018-2019 Annual Report. There are a couple of key pieces of information we should keep in mind.
Nearly all of the detected influenza was Influenza A (about 95%)
Compared to prior 5 flu seasons, this season
Started 5 weeks earlier
Lasted 6 weeks longer
Of all the testing administered, percent positive peaked at around 30%
What about 2020-2021?
The most recent flu season report is so mind-boggling that we should just dive right into it - you be the judge!
The first sentence of the Abstract from the 2020-2021 summary report:
During the 2020-2021 Canadian influenza season, no community circulation of influenza occurred.
A grand total of 69 laboratory-confirmed cases of influenza virus was reported for the whole season. Did they just under-test for influenza?
No. Actually, fuck no. Between 2014 and 2019, the average number of tests administered per season were between 237,777 and 391, 862.
How many tests were administered in 2020-2021? 632, 580. Nearly twice the average. With 69 confirmed cases, that is a test positivity of 0.01%.
To drive the point home:
In 2020-2021, Canada administered nearly twice as many tests for influenza, and concluded there was no community circulation of influenza.
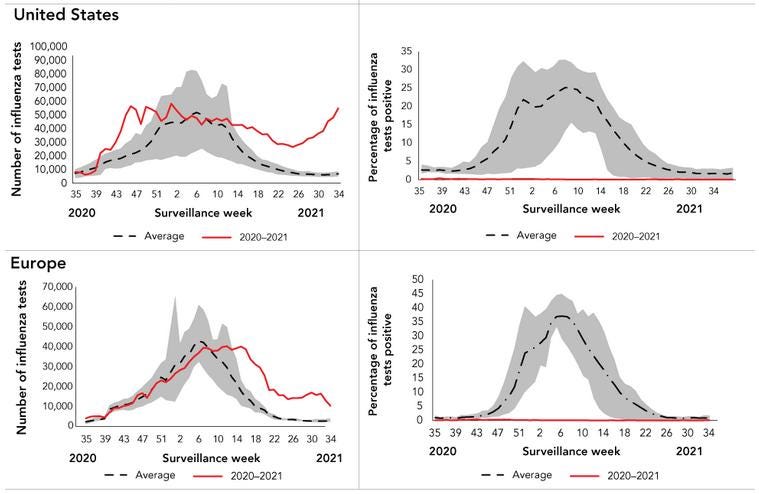
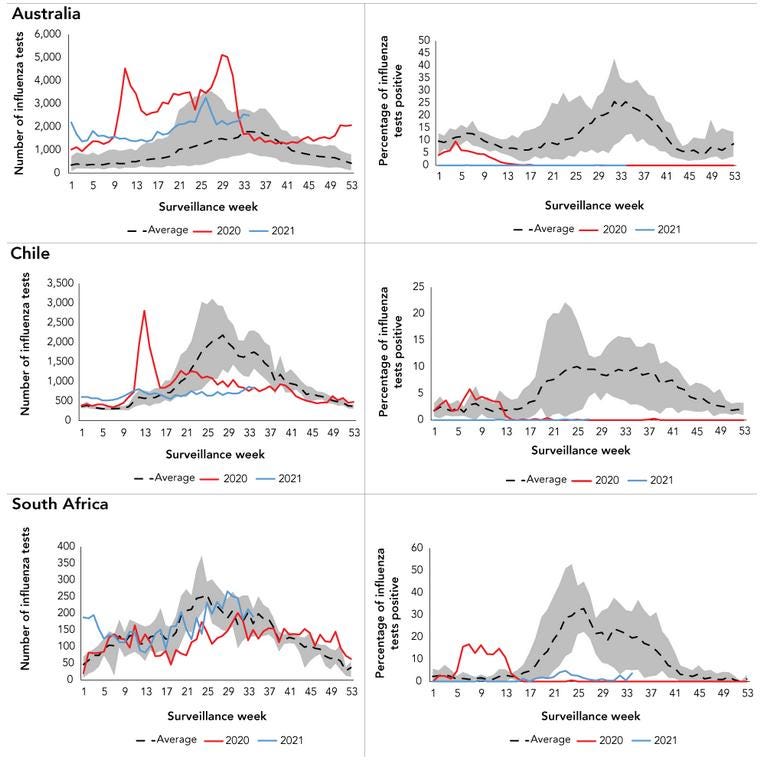
What about the rest of the Northern hemisphere?
Ok, how about the Southern hemisphere?
The Problem:
The Flu had gone nearly extinct for the whole season of 2020-2021 - epitomized by the Canadian data - and we don’t have a convincing explanation.
Where Did the Flu Go?
Typically, when you present this information to “Experts” they have two ways of blowing it off.
Our non-pharmaceutical interventions (lockdowns, masking, and social distancing) were so effective that it nearly eradicated influenza.
Viral Interference - inhibition of viral reproduction caused by previous exposure of cells to another virus.
Some of you may be thinking, if our lockdowns and masking efforts were so effective, then why was SARS-CoV-2 spreading so rapidly in the same time period? Yea, that’s a good question. A very good question.
Despite the fact that we’ve known for years from pandemic preparedness literature that lockdowns and masks (except N95) do fuck-all for preventing the spread of an airborne respiratory pathogen, this did not stop the CCDR from using this cop-out.
…non-pharmaceutical public health measures (i.e. school closures, travel restrictions, mandatory masking and increased handwashing)…throughout the 2020–2021 flu season…have shown that these measures were effective in reducing the incidence and impact of influenza in Canada.
Canadian “Experts” are not alone in this - here’s an article from The Lancet, in which the authors make the same brilliant deduction.
What about Viral Interference?
Viral interference is a rather complex problem, one which would require a whole other blog post to explore. But, this and that should get you started on the path of understanding just how hairy this is.
However, for the sake of argument let us accept the principle of viral interference as stated in the literature. In our case, the explanation goes something like this…
Infection with SARS-CoV-2 in some complex immune-mediated pathway is preventing the syndromic infection by Influenza, so we don’t see many cases of the Flu
The above statement relies on the following assumption:
Influenza and SARS-CoV-2 have a negative interaction - such that infection with one virus prevents infection with another
What if the opposite is true? What if infection with one enhances infection with another?
This is called Superinfection
Superinfection is when a second infection occurs in the setting of an initial infection.
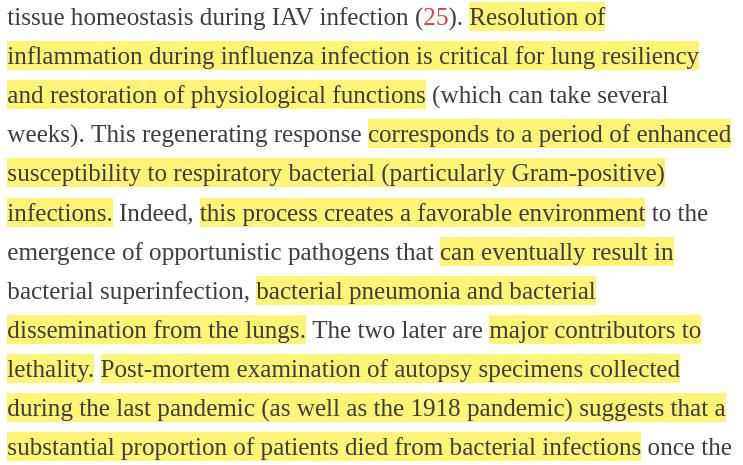
Using Influenza as an example, here is a great article summarizing the characteristics of infection and repair, as well as the potential for superimposed secondary infections.
The article goes onto suggest mechanisms…
Influenza A (IAV) disrupts the functions of respiratory barriers
Leads to exposure of new attachment sites
IAV can alter respiratory ciliary function
Impairs clearance of pathogens from lungs
Alternation of innate immune response secondary to IAV infection
leads to loss and/or dysfunction of macrophages and neutrophils
The Case for Viral Superinfection
What do we know about the people who get so sick with COVID-19 that they get hospitalized or die?
At this point, it should come as no surprise to you, dear reader, that the highest predictor of poor outcomes with COVID-19 pneumonia is age and comorbidities.
Which means that the elderly and the metabolically unhealthy tend to suffer the most, by a huge margin.
Let’s conceptualize this problem thus:
A person who is old (senescent) or metabolically unhealthy (comorbidities) will have a relatively frail or ineffective or slow immune response to an infection
this is one way in which COVID-19 outcomes can be modulated
A person who has another infection (in addition to SARS-CoV-2) similarly has a weakened or exhausted or otherwise preoccupied immune system
this is an analogous way in which COVID-19 outcomes can be modulated
Now, I’m not suggesting that all severe COVID-19 is due to influenza alone. No.
What I am saying is that it’s possible that in people who have severe COVID-19 infections, there is a likelihood that a co-infection with another virus, bacteria, or fungus is contributing to the poor outcome. Similar to how a person who is obese, diabetic, and elderly or frail may contribute to their poor outcomes.
In my own personal experience, during the Spring of 2020 surge in admissions and deaths in our hospitalized patients, rarely would someone be admitted just for COVID-19 pneumonia. Almost all of them were elderly, an overwhelming majority had comorbidities, and in my estimation a majority of poor outcomes was associated with other co-infections (bacterial and fungal included).
To keep this kosher, let’s take a look at a relatively early paper that explored this issue.
How does Influenza contribute to COVID-19 outcomes?
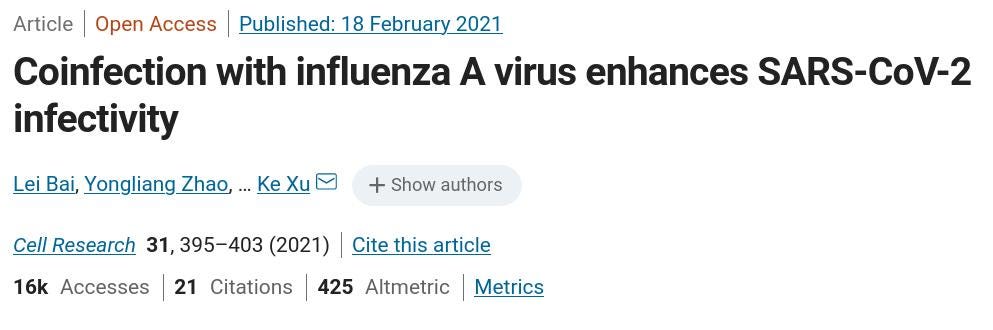
Everything we’ve discussed above led me to this article, and boy is it damning.
In this study, the authors performed a rather thorough examination of how infection with IAV could affect superimposed infection by SARS-CoV-2. Let’s get right into.
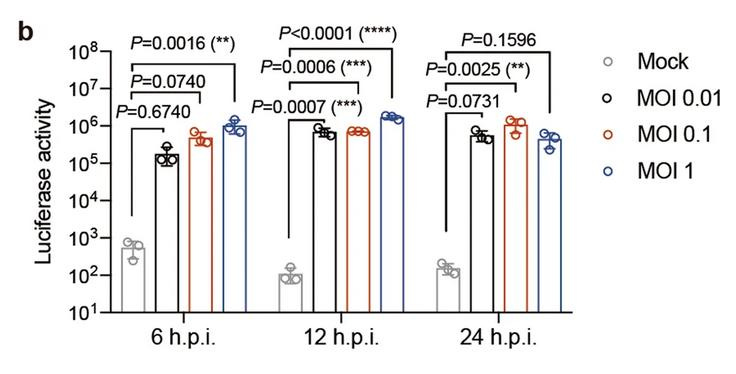
The authors used cultured cells (e.g. alveolar basal epithelial cells - lung tissue) and mice model to study the interactions.
Key: One cell line used (referred to as A549) is susceptible to IAV but not SARS-CoV-2 infection.
Finding #1: IAV promotes SARS-CoV-2 Infection
*Pseudo-SARS is a version of SARS-CoV-2 that is tagged with a reporter (e.g. Luciferase) such that the authors could determine if SARS-CoV-2 had infected the cells.
Fear Not: They also did this with live SARS-CoV-2 to validate the finding…
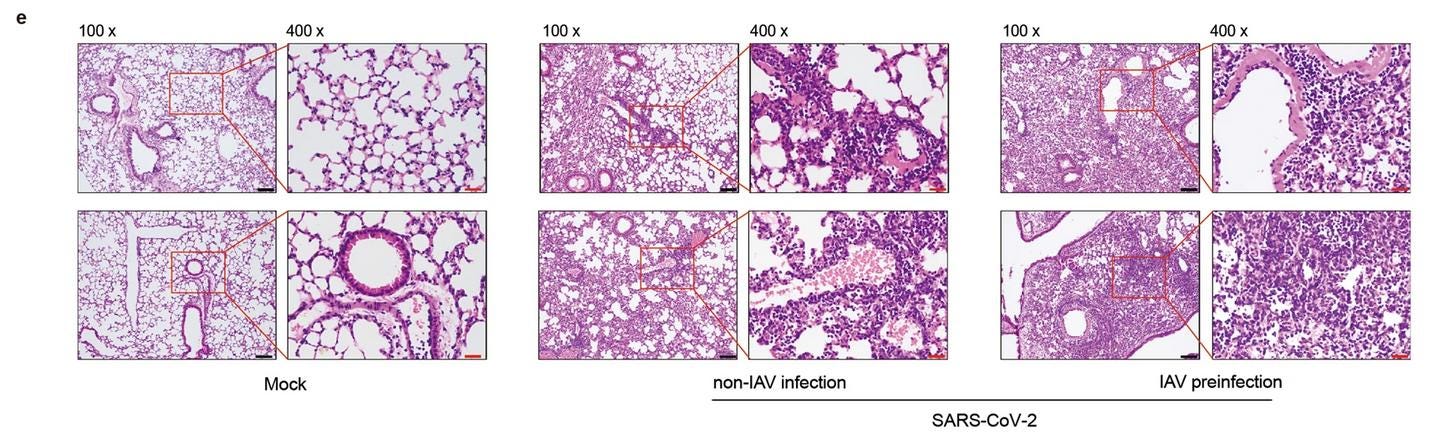
Finding #2: IAV and SARS-CoV-2 co-infection in mice results in higher viral load and more severe lung damage
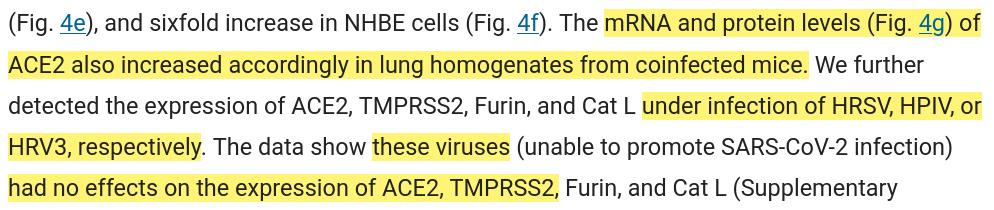
Finding #3: Interaction between IAV and SARS-CoV-2 is unique from other common respiratory viruses
Surely, this interaction could not be unique to Influenza A + SARS-CoV-2. So the authors tested this hypothesis…
HRSV - Human Respiratory Syncytial Virus, HPIV - Human Parainfluenza Virus, HRV3 - Human Rhinovirus 3
Finding #4: IAV induces elevation of ACE-2 expression
You may have heard about the relationship between SARS-CoV-2 and ACE-2 receptor binding. Well, it’s a big deal. It may very well be that this interaction is responsible for far more than just invasion of respiratory epithelial cells. Would recommend the work of @Parsifaler for more insights.
Additionally: ACE-2 levels increased 28-fold in A549 cells co-infected with IAV and SARS-CoV-2
This relationship was also found on histologic examination of mice that were co-infected:
IMPORTANT: When ACE-2 expression was knocked-out in another cell line, the enhancement between IAV and SARS-CoV-2 was completely abolished.
Finding #5: IAV Gene segment 2 stimulates SARS-CoV-2 Infection
Segment 2 encodes for a protein called PB1, which showed the greatest effect on both SARS-CoV-2 infectivity as well as ACE-2 expression. PB1-F2 is a pro-apoptotic factor which also regulates innate immunity. PB1-N40 contributes to viral pathogenecity.
Nuff said.
The Cherry on Top: PCR Testing
In an earlier twitter thread, I explored some odd documentation regarding the ability of PCR testing to discern and report infection with either SARS-CoV-2 and Influenza A/B - or, lack thereof.